Of all fungal diseases, mycoses (fungal lesions) of the skin on the feet are the most common. They are also called ringworm or athlete's foot. About 30% of the population have problems with fungal diseases. Almost half of patients never take them to the doctor and spread the fungus among loved ones. Microscopic pathogens invade the dermis (skin) or nails. In the latter case one speaks of onychomycosis.
Why are the feet most commonly affected?
Various fungi are always present on the skin. Their reproduction is inhibited by beneficial bacteria and skin secrets. With violations of immunity, shifts in the composition of the skin microflora, a favorable time arises for fungi - they are free to multiply. Entrance gates for infection can serve as periodic damage:
- Scratch;
- cracks;
- Scrub.
Another cause of mycoses are endocrine disorders. With disturbances in the work of the endocrine glands, not only the hormonal balance changes, but also the work of the whole organism. Among other things, the composition of the skin secrets changes, as a result of which they lose their bactericidal properties. Fungi can feed on it, which also promotes reproduction.
Other factors also contribute to the weakening of protective forces:
- alimentary exhaustion (malnutrition);
- avitaminosis;
- excessive physical and psycho-emotional stress;
- concussions;
- regular stress.
All of these are non-specific causes of skin fungal lesions. They can cause athlete's foot, smooth skin on the body or mucous membranes.
In addition, there are special species of fungi (genus Trichophyton or Microsporum) - pathogenic (pathogenic). When in contact with the skin or on its surface, they cause disease. In the case of the feet, the disease is known as rubromycosis. On the body, these pathogens form specific spots - lichen. You can get infected from a person or animal.
The skin of the feet is a special place for fungi. There are always many keratinized cells. Microbes serve as housing and food. "Rampant" fungus contributes to sweating of the feet. In closed shoes, a nutrient-rich, moist environment forms on the feet - the "dream" of every fungus. If a person neglects foot hygiene, does not dry and disinfect shoes, then the infection first multiplies in them, and then passes to the feet of the "owner". Poor hygiene products, dryness, synthetic socks also contribute to the spread of a fungal infection.
Signs of a fungus, visually perceptible
Treatment of dermatomycosis is easier the earlier the disease is diagnosed. In advanced cases, therapy is long-term, it involves taking pills and using external funds. In the early stages of mycosis, ointments can be dispensed with. It is important to be able to recognize the early symptoms of the fungus in order to see a doctor in time.
How the fungus looks depends on the form of mycosis. Fungal infestation of the feet can occur in 3 different variants, as well as in a mixed form - if there are signs of three main types on the legs at the same time.
intertriginous form

A type of tinea pedis that primarily affects the skin between the toes. The first symptom of the disease is the appearance of a painful crack between the 3rd and 4th or 4th and 5th tires of the foot. The damage is small, but causes inconvenience when washing feet and walking.
If you carefully examine the wound, a whitish border around it is noticeable (example in the photo). This is what the edges of the skin around the detached tear look like. The sore can itch, ooze, increase, or vice versa - periodically heal, and then reappear.
In some cases, the crack heals, but the skin continues to shed, hyperkeratosis (thickening of the dermis) develops, corns and calluses appear. With the advanced intertriginous form, the cracks become larger (example in the photo), appear between other fingers, the skin constantly gets wet. It is difficult for the patient to move and wear shoes.

As this form progresses, the crack increases in size. Similar signs appear on the second foot. Thick and large layers of skin peel off around the wound. The second (attached) end does not shed and attempts to remove the keratinized portion with fingers result in additional damage to the foot.
This type of athlete's foot is the most common. The manifestation of the pathology is initially not accompanied by any symptoms. As a rule, the infection develops between the 3rd and 4th fingers and does not change the color and texture of the skin until a certain point. After that, wet cracks and layers of skin appear.
The foot itself is unharmed, but when the fungus is infected, the feet can sweat more than usual. Therapy of the fungus of the intertriginous form is characterized by medium complexity.
dyshidrotic form

In this form, the first signs of a fungus on the skin are blisters on the arch of the foot. Most often - near the heel. The surface becomes dry, deep seals appear (like nodules to the touch). Later, they noticeably rise above the level of the skin, as they are filled with fluid. Vesicles (vesicles) are usually small - from 2 to 5 mm in diameter. They can merge, forming larger ones - bullae. Other symptoms include pain and itching around the rash.
The progression of the dyshidrotic form of mycosis is manifested by the bursting of bubbles. In their place, small or large erosions are formed. Often they become infected with bacteria and begin to boil. Erosions do not heal for a long time and make walking painful. In some cases, erosion disappears, and in its place there is aridity.
scaly shape

As the disease progresses, severe hyperkeratosis develops on the feet. The size and number of cracks increase. The biggest can bleed. Such damage is the way for other pathogenic microbes to enter the body. Therefore, the wounds periodically become inflamed, abscess can form. The most common form of athlete's foot is manifested by increased dryness of the skin on the plantar part of the limb. It can mean a recent accession of the fungus, or vice versa - be the result of the development of other forms.
At the arch of the foot and in the middle, the dermis becomes dry, thin, shiny and covered with a network of furrows. Hyperkeratosis is observed in the area of \u200b\u200bthe fingers and heels - rapid keratinization, during which dead particles do not have time to detach. Calluses or corns form on the forefoot. There are small tears on the heels. The entire surface is rough from severe flaking. The patient may experience itching. With prolonged development of mycosis, this symptom is absent.
You can identify the fungus on the legs by excessive dryness, unpleasant odor, itching and constant peeling of the skin.
onychomycosis
Onychomycosis is a type of fungus of the foot (or palms) that affects the skin appendages - the nails. Nail fungus can be caused by the same pathogens that cause skin mycoses. You get infected with mold and other types of monofungi in manicures, on the beach, when trying on new shoes on your bare feet, when going to the sauna or swimming pool. An ingrown toenail can be a contributing factor. The thumb is most commonly affected.
Upon hitting the nail plate, the fungus begins to divide. It penetrates deep into the nail and spreads over its area. The first signs by which you can identify the fungus in the nails are the loss of shine, the appearance of spots (white, yellow, brown, greenish) and a change in the shape of the nail plate.
As the disease progresses, the structure of the nail in the discoloration zone changes (it thickens, becomes bumpy, loose).
Runny fungus on toenails looks like thick yellow growths. It is difficult to care for the affected nail plates. Before each trimming, you need to do hot foot baths. After contact with water, nails become softer and easier to remove with manicure tools.
If the nail fungus is not treated, onycholysis begins - the plate completely or partially flakes off. After removing its remnants, the nail does not always grow back. Sometimes the process of detachment ends with a complete loss of nails.
General principles of treatment
The fungus on the feet is treated with ointments, creams, solutions, special varnishes. In parallel, the patient is prescribed antifungal drugs.
For the entire period of treatment, careful foot hygiene, weekly cutting and sawing of the damaged part are shown. Every day the patient has to use a pedicure file to remove the keratinized cell layer from the surface of the foot.
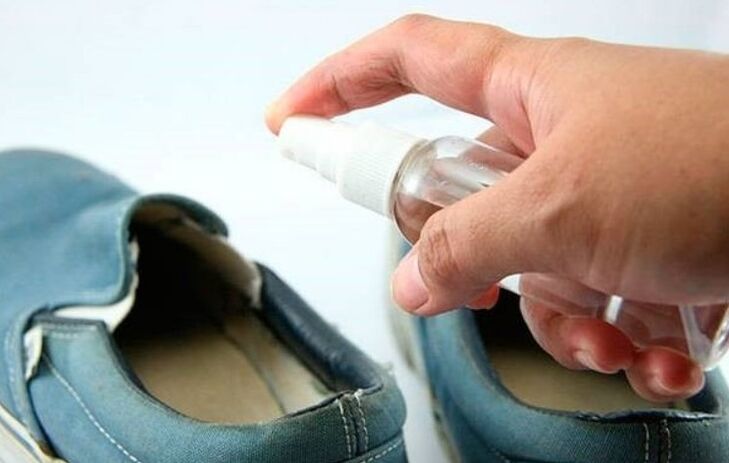
It is also important to carefully care for shoes - treat them with antifungal drugs or disinfectants. Shoes are dried and aired in the open air every day.
External Funds
At the initial stage of athlete's foot, only ointment or cream is prescribed. For treatment, a cream and other drugs are prescribed. They are applied to the skin 1-2 times a day after washing the feet thoroughly with a simple soap. Before using creams, it is important to dry your feet completely. Do not apply medication to wet skin. After the treatment, the patient should wear cotton socks.
tablets
It is impossible to treat the fungus yourself with pills. All drugs adversely affect liver and kidney function and have a number of contraindications. Before prescribing treatment with antifungal drugs, the specialist recommends a general and biochemical blood test, which allows to assess the condition of vital organs.
preparations for nails
Useful in the treatment of onychomycosis and athlete's foot. In the first case, they are used to remove the affected part of the nail, in the second - to prevent infection of the nail plates with fungi.
It is most convenient to be treated with varnishes - they are applied to the nails 1-2 times a week. The cheapest medicines for nail fungus are solutions that are applied to the nails twice a day until full recovery. Special gels are popular. They visually improve the condition of the affected nails, and they also stop the fungus from multiplying. Ointments are also prescribed for onychomycosis. They are applied to the affected plates in a thick layer, covered with a bandage and kept like this until the product is completely absorbed. The treatment is repeated twice a day.
Preventing athlete's foot is much easier than treating it. To do this, you need to lead a healthy lifestyle, take your own slippers to the pool and sauna, regularly wash and air your shoes, wear socks made of natural fabrics, use anti-sweat products. With regular visits to "wet" institutions, you should use antifungal drugs prophylactically - treat the skin of the feet 1-2 times a week.


















